The post Genesis Clinic gets official ‘Mother-and-Baby-Friendly’ status appeared first on All4Baby.
]]>“This is a great accolade for us, and a real endorsement of natural, active birth,” says Jude Polack, director and founder of Genesis Clinic. “There are those in the local medical fraternity who believe that by helping moms deliver naturally, we are taking the riskier route. Instead they claim that Caesareans and medical intervention are the safer method of giving birth. Based on a vast quantity of global research, however, WHO and UNICEF have declared that natural birth is the safest for both mom and babe, which is a significant reassurance for our clients.”
Genesis Clinic has achieved its Mother-Friendly status thanks to its pro-mom labour and birthing practices. “We view labour and birth as a natural process,” says Polack. “It’s all about giving moms the freedom to follow their instincts, while supporting them with sound and safe birthing procedures.”
This means giving mom unrestricted access to birthing companions, encouraging her to eat and drink during labour, and giving her the freedom to walk and move about, as well as assume whichever position feels most natural to her for the birth, provided there are no complications.
The Clinic also discourages medical interventions, and offers natural pain control such as massage and nitrous oxide. “In emergencies however, we have obstetricians and gynaes on stand-by, as well as a fully equipped operating theatre should the need arise,” says Polack.
For the Baby-Friendly part of its accreditation, Genesis Clinic adheres to 10 steps for supporting and maintaining successful breastfeeding. “For us, breastfeeding is simply an extension of our philosophy about birth – that it’s a beautiful and natural process which most women embrace instinctively if given the right support and encouragement,” says Polack.
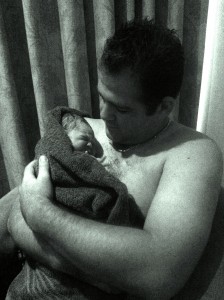
So, for instance, babies are placed skin to skin with their moms immediately after birth, and moms are helped to recognise when their newborns are ready to breastfeed. “We also encourage breastfeeding on demand, which is made easier at Genesis because all babies room in with their moms throughout their stay with us.”
All of which means happy, and most importantly, healthy babes and moms… and a big thumbs-up from WHO and UNICEF.
For more information, visit www.genesisclinic.co.za
The post Genesis Clinic gets official ‘Mother-and-Baby-Friendly’ status appeared first on All4Baby.
]]>The post Get the birth you want! appeared first on All4Baby.
]]>That’s because in South Africa’s private healthcare arena, the decision to ‘go natural’ is often one that moms have to rigorously defend. Based on the experiences of moms who come to us at Genesis Clinic after being discouraged by their doctor against natural birth, there are three clues to alert you to the fact that you’re dealing with a potential medical bully.
The first is a doctor who warns you that your baby is too big or that you’re too small to deliver naturally. They’ll start hinting about this early on, preparing moms for a change of game plan. “Just start getting your mind around the possibility that you might need a Caesarean,” they’ll say. But the doctor who tells you early in your pregnancy that your baby is going to get stuck is flat-out lying to you.
There is no way to tell, even from an x-ray, that a woman’s pelvis won’t distend and disengage sufficiently for her baby, and ultrasounds can be off by as much as 400 grams. In my practice, I’ve seen tiny women giving birth without trouble to babies over 3.5 kg, while bigger moms needed help delivering babies just over two kilos.
Another common sign of medical bullying happens quite late in the pregnancy, at about 36 weeks. The doctor will start priming you that your baby hasn’t engaged or dropped down, which will unfortunately necessitate a Caesarean. A large percentage of babies however, will only engage once labour starts, particularly in second pregnancies; in fact, most second or third babies will only engage the day before or even once labour has started.
The third clue you have a medical bully on your hands is when your doctor tells you halfway through your pregnancy that your amniotic fluid is drying up or calcifying; this typically only starts to happen though, once mom is two to three weeks overdue.
We’re being deceived
To put it bluntly, women in South Africa are being deceived. They’re being given one-sided information aimed at pushing them into making decisions that suit the medical fraternity, which, in the case of private healthcare in South Africa, is significantly skewed towards performing C-sections.
The World Health Organisation says that a Caesarean rate above 15% is unjustifiable, yet private hospitals in South Africa have rates as high as 68% (National Perinatal Mortality and Morbidity Committee Triennial Report, 2008-2010).
Disregarding elective C-sections, why is the rate so high? People joke and say that doctors in South Africa do Caesareans so that they’re not interrupted on the golf course. Convenience does, of course, come into it, but it’s more complex than that.
Did you know that gynaes and obstetricians pay upwards of R40 000 a month on medical insurance, a premium that goes up significantly should insurance have to pay out for malpractice.
It’s understandable therefore, why some doctors would rather do a hundred unnecessary Caesareans than risk losing one baby or mom in a real emergency. For these doctors, C-sections seem like the safest obstetric procedure from a legal standpoint.
Currently, government is working on capping medical malpractice payouts, which might well have a significant impact on the number of C-sections pushed onto unwilling women in years to come. Until then though, what can moms do to get the best chance of having the safe, natural birth they want, without the bullying?
Getting the birth you want
If you want to give birth naturally, the most important thing you can do is start off with the right caregiver. From the very beginning, have an in-depth discussion with your doctor. Find out what his or her C-section rate is, and what his or her philosophy about natural birth is. Arm yourself with information about the pros and cons of both routes; don’t just rely on what you’re told.
If your doctor is clearly not on the same page as you, then you should consider finding a new caregiver. I’m always amazed how moms will swop hairdressers and nail technicians and insurance companies if they’re not getting the service they want, but they’re terrified of changing doctors.
This is a very special time in your life; it’s your right to find a caregiver who will help you to enter motherhood in the way you choose, while safeguarding both your and your baby’s life.
You should also consider finding a midwife or doula, even if you are planning to give birth in a hospital. They will come to your appointments with you, support you and stand up for you, while ensuring you get a safe experience.
Currently, private hospitals don’t allow midwives to come into the labour room with moms, and only a handful allow doulas; with consistent pressure from moms however, this will change. Women need to put pressure on hospitals and doctors to start offering them the birthing experience they want. There is no reason why all hospitals shouldn’t have active birthing units, giving moms the beautiful experience they so want, with the safety net for the 10-15% of moms who’ll experience complications.
I always remind women that this isn’t just the day that a baby will be born … it’s also the day that a mom is born. This is a huge rite of passage for a woman; she should be allowed to make this journey in the way she chooses, and with a caregiver who is mindful not only of mom’s and baby’s safety, but also of her hopes for how she wants to bring her child into the world.
For more information on Genesis Clinic, visit: www.genesisclinic.co.za
The post Get the birth you want! appeared first on All4Baby.
]]>The post Water birth: My real life story appeared first on All4Baby.
]]>Curious, I started to research it and found only positive information…
A calm experience
The most positive piece of information that I could find, was that birth for the infant was a traumatizing experience but when a child is brought into this world through a water birth, the experience is less traumatizing. This is because the infant goes from water in the amniotic sac, through the birth canal, into water again.
The water that the infant is birthed into has a calm and soothing effect. The researched I did also suggested that this will also make for a calmer child.
Pain management
Another huge plus is that waterbirth assists in pain management. I wanted to go natural as I am scared of hospitals and injections. I would rather experience the pain of an active birth than have an epidural or a c-section.
An individual, rather than a patient
I wanted to be an individual, not a patient with a medical condition which nurses treat as it’s their job. I wanted someone who is passionate about birth and babies to take care of me.
The more I researched water birth, the more I knew in my heart that this was the route I wanted to go.
The best of both worlds
Once I had decided on a clinic, I chose a gynaecologist and a midwife I felt comfortable with. They were both affiliated with the clinic that I had chosen.
I got to have the best of both worlds, as I saw the gynaecologist regularly and had my midwife on standby at all hours of the day. I messaged her on a regular basis and she always responded to all my silly questions and worries.
By the time I was ready to give birth, I knew my midwife personally and we had a great relationship. She knew what kind of experience I was looking to have and made it her mission to give it to me.
My birth story
The morning my water broke, I phoned my midwife immediately. She was calm and shared my excitement.
Researched suggested that labour for a first time mom who has chosen active labour could be anything from eight to 24 hours. So we had plenty of time. Or so we thought.
My midwife told me that I could wait at home, where I was comfortable, until my contractions were three minutes apart for at least an hour.Only at that point, would I need to make my way to the clinic where she would be waiting for me.
I downloaded an application to time the contractions. It started slowly, and could be timed at 15 minutes apart for a few seconds each. After about an hour it escalated to six minutes apart, lasting for about 30 seconds each.
Suddenly, I couldn’t determine where one contraction started and were one ended. It was just one big pain, which confused both my husband and I.
My mother kept advising us that we would need to make our way to the clinic. But, they had taught us at prenatal classes, that the husband should wait until the wife is ready to go to the hospital, as she will tell him – there is no need for the husband to force it. So, not knowing any better, my husband stalled our trip to the hospital, waiting for me to give him the go-ahead.
In the meantime, my pain continued to increase. I couldn’t talk nor could I comprehend how I was going to make it to the clinic which was about 20 to 30 minutes away. So, I kept quiet and dealt with the pain.
Suddenly, my pain changed. The intensity dissipated and I jumped up exclaiming that we had to leave.
I couldn’t sit normally in the car, as I was in too much pain. I pushed the back of the seat down and kneeled down on the front seat. I could tell that my husband was speeding but it still felt like we took forever to reach the clinic.
On our way to the clinic, my body felt the urge to push and I did. I couldn’t resist it or stop it. I thought this was the norm as I was so early in the labour process. When we stopped at the clinic, the staff was ready for us and my midwife led me to the room that they had reserved for me.
The midwife examined me and uttered to my husband and her staff that I was fully dilated. She looked at me, smiled and said: “Your baby will be here in a few minutes. It’s time to get into the water.”
The staff was so efficient and knew exactly what needed to be done. One of the midwives on duty stood behind me and massaged my back. It took all the pain away.
Within a few minutes I was in the water and pushing. The warmth of the water calmed my pain. My midwife guided me as to when I should push and when I should stop. This assisted in a gradual birth and thus I did not experience any degree of perineal tearing.
My husband assisted the midwife in pulling our son, Vincent out and he was also given the opportunity to cut the umbilical cord once it had stopped pulsating.
When I took him out of the water, he did not cry. He was perfect and so happy. He laid on my chest and I couldn’t stop kissing him. He only cried when they took him away from me to weigh him. The moment they brought him back to me, he stopped crying again.
Breastfeeding assistance
My birthing clinic encourages moms to breastfeed and spent hours with me until I was comfortable and Vincent had latched properly.
It was the most amazing feeling to know that my body supplied Vincent with nourishment.
A love for water
At home, when Vincent is unsettled for some reason and I can’t settle him, I put him in a nice warm bath, keeping only his nose outside of the water. He falls asleep like this or becomes extremely calm and settled. He loves to bath and he loves water. Because of his birth experience, I believe water is now his comfort.
An experience I would go through again
My birthing experience was so positive, I will not hesitate to do the exact same thing again. I would also recommend a physiological birth (100% natural without any medical intervention, including pain medication) to any mom-to-be.
It’s well worth the experience.
For more information on natural and water birth, visit Genesis Clinic www.genesisclinic.co.za
The post Water birth: My real life story appeared first on All4Baby.
]]>The post Perineal tear: The lowdown on tearing down low! appeared first on All4Baby.
]]>When baby’s head crowns during childbirth, the tissue around the vaginal opening can tear. Typically, tears range from mere skin snicks which heal on their own after childbirth (called first-degree tears), to tears involving vaginal tissue and the perineal muscles, which will need a few stitches in the delivery room (second-degree tears). Far more rare are third- and fourth-degree tears, involving the vaginal tissue, perineal muscles, anal sphincter and at worst, tissue within the rectum. These tears require repair in theatre.
Sounds painful
Understandably, moms delivering vaginally are often concerned about the pain of tearing. The good news is that you are unlikely to feel the tear during labour, since the skin is stretched taut, making it quite numb.
Afterwards however, pain will vary depending on the severity of the tear; in most cases, since the majority of tearing is either first- or second-degree, moms report stinging rather than actual throbbing pain.
Will I definitely get a tear?
The only delivery where a wound is a certainty is a Caesarean section. For a natural birth, the chances of going home with a tear are significantly smaller: around 40% for first-time moms, and 20% in subsequent deliveries, with only 0.6%-0.9% of vaginal deliveries resulting in a severe tear, according to James, Steer, Weiner and Gonik in “High Risk Pregnancy Management Options” (2005, Saunders Elsevier).
What increases my risk of tearing?
Baby’s size and position during the birth have a big influence. Babies who are large for their gestational age or over 40 weeks are more likely to cause tearing. Risks also increase with babies born face first or facing mom’s front instead of her back, and with those who have a hand, elbow or shoulder protruding.
Mom’s position during delivery is another factor. The rate of perineal tearing is higher in a traditional hospital environment where moms are required to deliver on their backs, often with their legs in stirrups; this is a particularly bad position for tear prevention.
Medical intervention also significantly raises the risk, with forceps delivery probably the biggest culprit. Epidurals also have an impact, since they stop moms feeling the urge to push. Moms often end up pushing too early which can lead to a prolonged second stage of labour – a known risk factor in tearing – or they push too hard before the perineum has stretched sufficiently.
An augmented labour, where labour is helped along by drugs, further ups the risk. Contractions are often stronger than normal, which can cause the baby to crown too early and quickly.
My mom says I should have an episiotomy rather than risk tearing. Is she right?
This used to be the accepted thinking, but experience has shown that episiotomies, where the perineum is cut by the doctor or midwife, do not reduce the severity of tearing. In fact, an episiotomy increases the risk of having a more severe third- or fourth-degree tear. Just think how hard it is to tear material, yet if you make a little nick, the fabric rips easily; the same happens with an episiotomy.
A perineal tear is usually only superficial, running through the skin, whereas an episiotomy cuts right through skin and muscle. This means episiotomies are usually more painful and slower to heal since they’re much deeper. The ragged edge of a natural tear is easier to match back if stitches are needed, so the wound heals with less scarring.
Episiotomies are only necessary in emergency situations when your baby needs to come out immediately, and there is no time to allow the perineum to stretch naturally.
How can I prevent a tear?
There is no way to guarantee that you won’t experience some degree of tearing during birth, but there are a number of ways to minimise the risk.
- Perineal massage in the last six weeks of pregnancy can help to soften and stretch the perineum. Ask your antenatal educator or midwife to show you the ropes.
- Emotional readiness for the birth is a big factor. If mom is ready and has done visualisations, then she’s not tense and stressed and her muscles are softer.
- If possible, deliver on your hands and knees, which is the best position since baby isn’t being dragged out against your perineum.
- Even if you aren’t allowed to deliver on your hands and knees, you can do a lot to ensure a slow, controlled second stage, which is probably the biggest factor in reducing perineal tears. Push very slowly and only when you feel a contraction, and resist doing ‘red-faced’ pushing. As the baby starts crowning, don’t bear down on the contraction. Your midwife or antenatal educator will guide you on this.
If I do tear, what happens next?
Second-degree tears will be stitched by your doctor or midwife under local anaesthetic, while third- and fourth-degree tears will be repaired in theatre.
Good wound care is important; ice packs will help reduce swelling and discomfort. Keep the area clean and don’t fiddle with the wound; salt baths are a great way to disinfect your wound while easing the discomfort.
If the wound stings when you go to the loo, pour warm water over the area while you urinate. You can also take stool softeners if it’s painful when you have a bowel movement.
Knowing all this, maybe it’s less risky to just opt for a Caesarean?
How you decide to have your baby is your personal choice, but remember that whether natural or by Caesarean, there is no pain-free, risk-free way to get a baby out of your body. Neither birth routes are without risks; both have their own set of associated problems which you should take into consideration.
While you’re weighing up your risks of getting a bad perineal tear, also weigh up your chances of having an infected C-section incision that will require surgical repair, which happens in around 4-8% of Caesareans. And while you might be caring for a wound if you give birth naturally, you’ll definitely be caring for one after a Caesarean.
For more information on Genesis Clinic, visit www.genesisclinic.co.za
The post Perineal tear: The lowdown on tearing down low! appeared first on All4Baby.
]]>